Innovation and sustainability of European healthcare systems
The EU health sector represents 10% of GDP, 15% of public expenditure and 8% of the workforce, and has high potential for innovation and growth. Impro
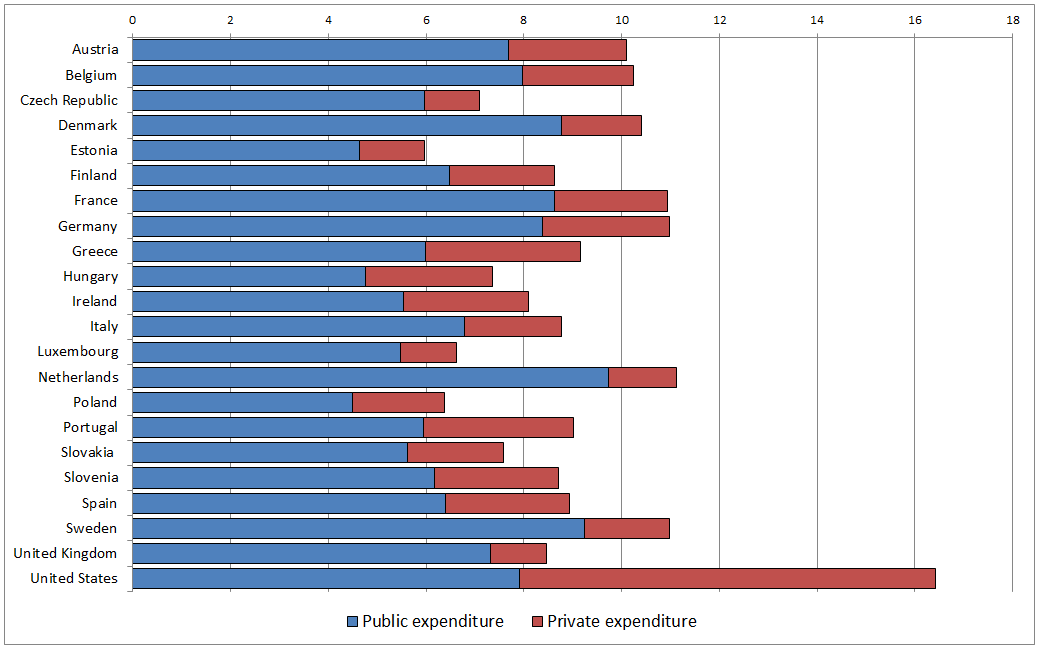
Health care expenditures
The cost of health care is expected to double by 2050 if reforms are not undertaken. This is being driven by a number of factors including demographics. With increased life expectancy and an ageing population in Europe, health care costs will rise. This includes the costs of the increased prevalence of noncommunicable diseases (NCDs), or chronic diseases, such as cardiovascular diseases, cancers, chronic respiratory diseases and diabetes.
The chart below shows health care expenditure as a percentage of GDP as well as the mix of public and private expenditure across many EU countries as well as in comparison to the U.S.
Health expenditure as % of GDP (2013)
Source: European Commission based on OECD Health Statistics
Technological advances in medicine, which can increase efficiencies in the healthcare system over the longer term, are increasing short term costs. Meanwhile, there are increased budgetary pressures on public funds putting further pressure on the healthcare system.
Projected public health and long-term care expenditure in the OECD countries as a percentage of GDP, in 2060
Source: Maisonneuve, C., and J. Martins. 2013. „Public Spending on Health and Long Term Care: A New Set of Projections.“ OECD Economic Policy Paper No. 6. Paris: OECD.
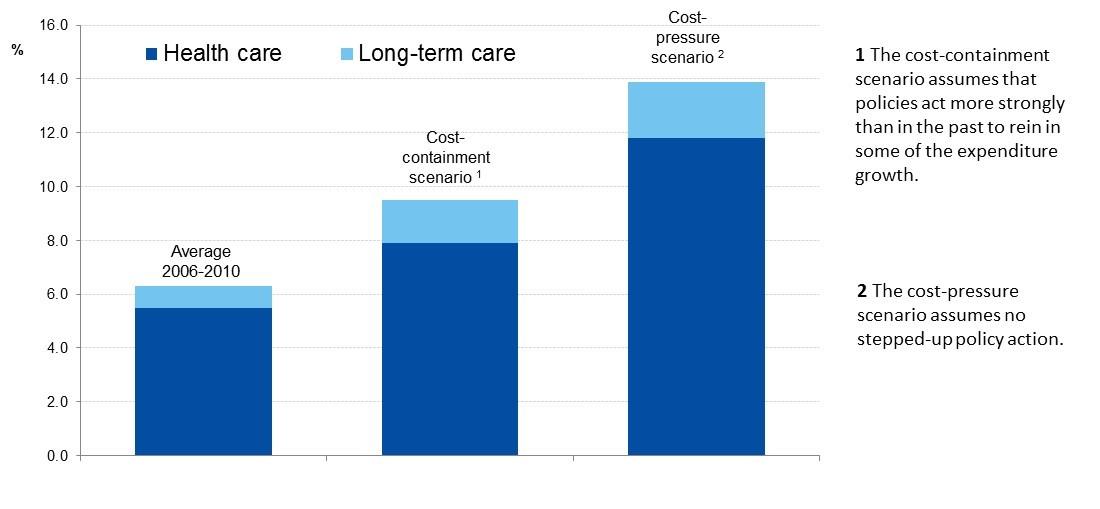
Cost containment efforts are not the answer. Healthcare systems in Europe need to be strengthened and modernized to be more effective and efficient. Healthcare systems need to provide higher value as well as greater access. In order to support and inform health system reform, smart investment and innovation in new technologies and the optimal use of existing ones, as well as in human capital, is critical. In this respect, economic analysis of the longer term impact of investment in healthcare is needed.
Focusing on health outcomes
Expenditure does not necessarily equate to better outcomes. In fact, there are significant differences in outcomes across as well as within countries. It is therefore important to understand the determinants of health. Big data can play an important role in the analysis of outcomes, not only in terms of health but also more broadly on social and economic outcomes. However, access to health data is limited and fragmented. Greater accessibility and transparency is need to maximize the value of existing data to enable learning about the impact of health care interventions.
In addition, more focus in needed on prevention, addressing health (proactively) not just diseases (reactively). Healthcare needs to be more patient-centered, empowering citizens to monitor and maximize their health. This requires a paradigm shift in the way healthcare systems are run as well as incentives. In a well-functioning health care system, the creation of value for patients should determine the rewards for all other actors in the system. Value depends on results, not inputs, therefore value in health care should be measured by the outcomes achieved, not the volume of services delivered.
Stronger partnerships required
Healthcare systems are complex and include a myriad of stakeholders who have conflicting goals such as access to services, profitability, high quality, cost containment, safety, convenience, patient-centeredness, and satisfaction. In order to overcome these challenges, building a better partnership between business, academia and regulatory authorities is essential. As a key economic and innovation-driven sector, health requires a predictable and fit-for-purpose regulatory environment conducive to growth, high-skilled jobs and higher global standards.
Today’s healthcare systems are ridge, input oriented and fragmented. While innovation is critical for the future of healthcare, there has been too slow an uptake due to barriers in the system. Silos needed to be broken down through stronger partnerships and multidisciplinary, integrated approaches to build future healthcare systems that are flexible as well as patient and results oriented.
The role of the EU
While healthcare system reform is the role of member states, the EU can support these efforts through stronger country assessment, benchmarking, reference networks, knowledge exchange and technical assistance. Through its 2014 communication, the European Commission outlined its plans to build more effective, accessible and resilience health care systems in Europe. This includes a set of activities such as health system performance assessments, patient safety and quality of care, integration of care and health technology assessments (HTA), which assess the ways science and technology are used in healthcare and disease prevention. However, more needs to be done to provide the appropriate incentives for healthcare system change as well as establish priorities for action.